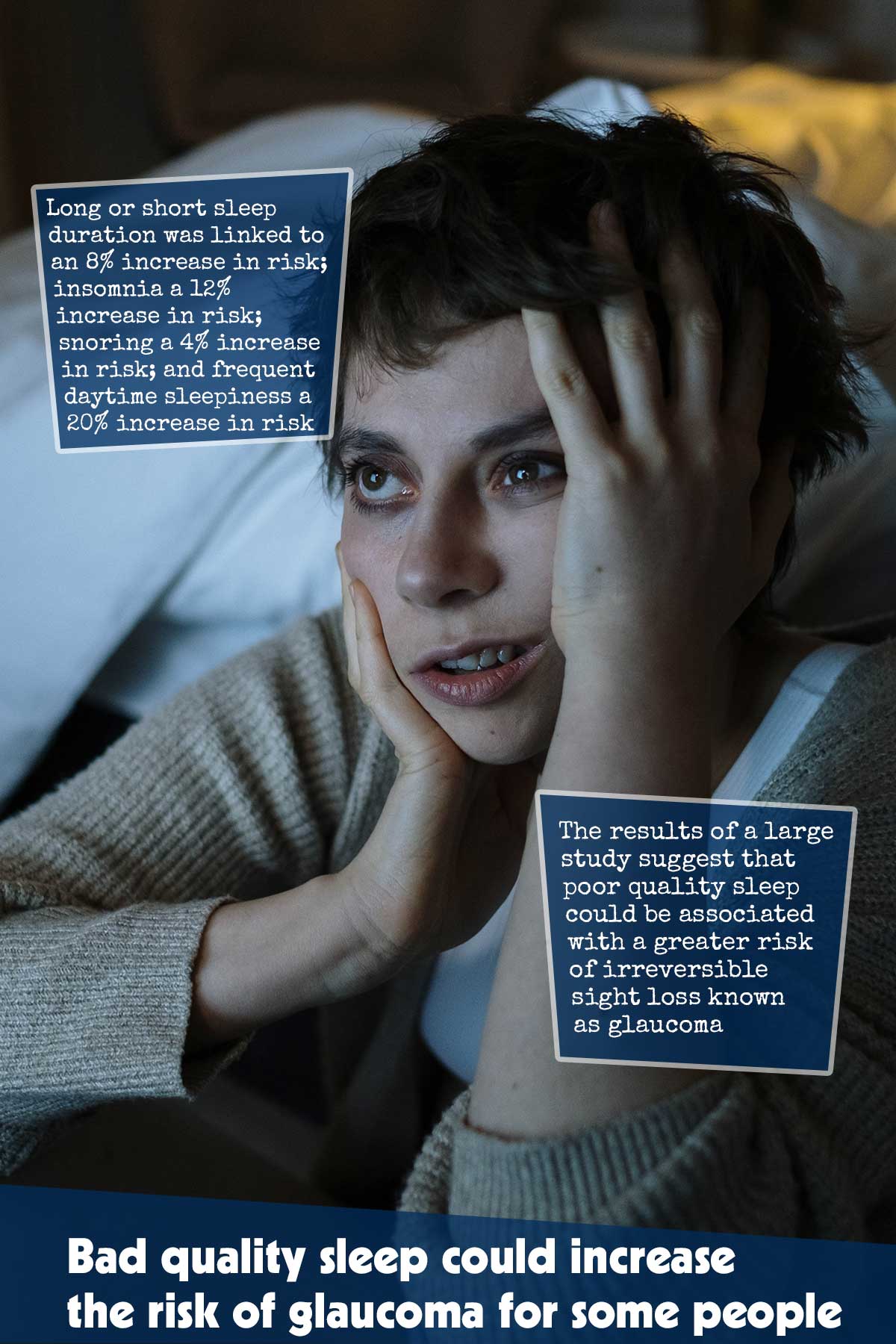
The results of a large study suggest that poor quality sleep, such as excessive or not enough sleep, snoring, and daytime sleepiness, could be associated with a greater risk of irreversible sight loss known as glaucoma.1✅ JOURNAL REFERENCE
DOI: 10.1136/bmjopen-2022-063676
The results emphasize the necessity for sleep therapy for individuals with a high risk of the condition in addition to eye checks for individuals with long-term sleep issues to monitor for early signs of glaucoma.
Glaucoma is a major cause of blindness which will probably impact approximately 112 million individuals globally by 2040.
Characterized by the progressive loss of eye cells that are light sensitive and optic nerve damage, the causes and factors that contribute to glaucoma are still not well understood. However, if left untreated, the condition can progress to blindness which is irreversible.
While screening at the population level might not be cost-effective, focused screening of groups with a high risk could be. And other studies suggest that sleep disorders could be a significant risk factor.
To look into these issues more in-depth, the researchers conducted a study to determine glaucoma risk in individuals with various sleep behaviors: insomnia; excessive or not enough sleep; owl (night) or lark (morning) chronotypes; snoring; and daytime sleepiness.
They made use of data from 409,053 individuals who participated in the UK Biobank, who were between the ages of 40 and 69 from 2006 to 2010 when they enrolled, and who had provided sleep behavior details.
Sleep duration of 7 to less than 9 hours a day was identified as normal and outside this range as not enough or excessive. Chronotype was classified based on whether the individual identified as more of an owl or lark.
The severity of insomnia, difficulty falling asleep at night, or waking up frequently, was categorized as sometimes/never or usually, while daytime sleepiness was categorized as never/rarely, occasionally, or frequently.
Background information on factors that could potentially influence the results was collected from the questionnaires completed when enrolled: lifestyle, age (an average of 57), race/ethnicity, sex, BMI, educational attainment, and residential area deprivation level.
Death registration data and medical records were made use of for tracking the survival and health of all the individuals until a 1st glaucoma diagnosis, emigration, death, or when the monitoring period ended, whichever came 1st.
Throughout a monitoring period of just more than 10.5 years on average, 8690 glaucoma cases were diagnosed.
Individuals with glaucoma were more likely to be a smoker, older and male, and to have diabetes or hypertension compared to individuals who weren’t identified as having the condition.
The other 4 sleep patterns/behaviors were all linked to varying levels of increased glaucoma risk except for the chronotypes.
Long or short sleep duration was linked to an 8% increase in risk; insomnia a 12% increase in risk; snoring a 4% increase in risk; and frequent daytime sleepiness a 20% increase in risk.
Snorers and individuals with daytime sleepiness had a 10% higher chance of having glaucoma in comparison to individuals who had a healthy sleep pattern, while individuals with a long/short sleep pattern and insomniacs had a 13% higher chance of having it.
Similar results were seen when categorized by various kinds of glaucoma.
Because this was an observational study, the cause could not be established. The study depended on self-reporting instead of objective measurement and reflected only 1 point in time. Glaucoma might itself impact sleep patterns, instead of vice versa.
There are however potentially credible explanations for the sleep disturbance and glaucoma association. The eye’s internal pressure, an important factor in glaucoma development, increases when sleep hormones are out of balance and when individual is lying down, as takes place in insomnia.
Anxiety and depression, which frequently go together with insomnia, could also increase the eye’s internal pressure, possibly due to dysregulated cortisol production.
It has also been suggested that prolonged or repetitive episodes of low cellular oxygen levels, due to sleep apnea, could result in the optic nerve being damaged.
As sleep behaviors are modifiable, these results emphasize the need for sleep treatment for those with a high glaucoma risk and potential ophthalmologic screening in people with long-term sleep issues to help in preventing glaucoma.