According to research, a weight-loss surgery commonly performed on obese adolescents as well as young adults is seen to have a detrimental impact on bone health.1✅ JOURNAL REFERENCE
DOI: 10.1148/radiol.223256
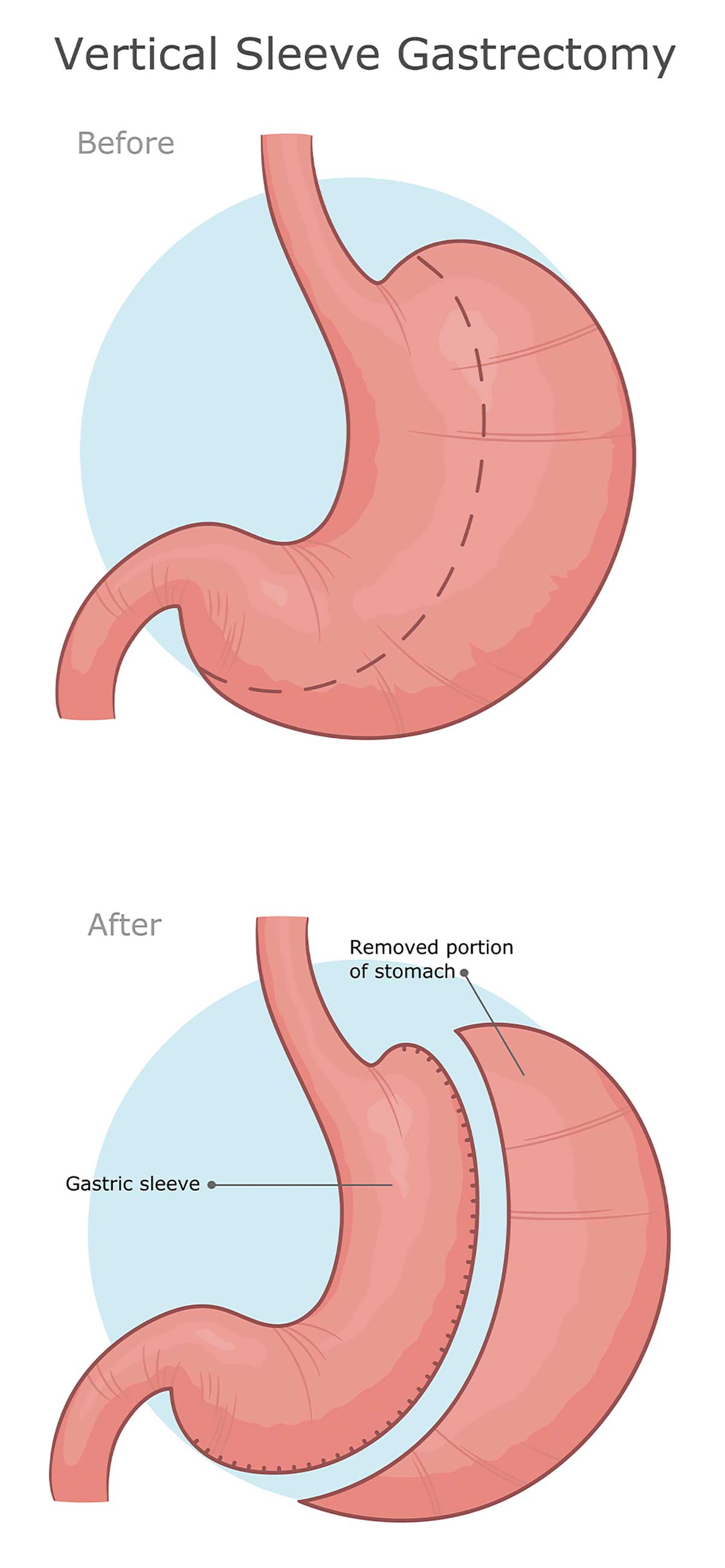
Childhood obesity is increasing and surgery for weight loss is an efficient method for reducing weight and improving cardiometabolic comorbidities. This study looked at the long-term impact that sleeve gastrectomy, the most commonly performed kind of surgery for weight loss, has on bone marrow fat and bone strength in adolescents and young individuals.
Sleeve gastrectomy removes about 75% to 80% of the stomach to limit food consumption and encourage weight loss. It normally creates a round stomach in the shape of a sleeve or tube.
The approximate number of sleeve gastrectomy surgeries carried out every year increased from more than 28,000 procedures in 2011 to more than 122,000 procedures in 2020. Gastric bypass has been overtaken by sleeve gastrectomy as the main weight-loss procedure.
Individuals between the ages of 13 and 24 years were enlisted from 2015 to 2020 for the study. The adolescents and young individuals were moderately to severely obese. The young individuals had a BMI of 35 or higher. A BMI of 30 or higher is regarded as obese. Adolescents participating in the study were at 120% of the 95th sex- and age-specific percentile.
Of the 54 participants, 29 were in the control group and 25 underwent sleeve gastrectomy. Forty-one of them were female. The group that had the surgery included individuals with a minimum of 1 co-morbidity related to obesity, or a BMI at or higher than 40. The control group was obese but didn’t plan to have sleeve gastrectomy but had exercise and dietary counseling.
Before the sleeve gastrectomy procedure as well as 24 months after, participants had blood tests, a physical examination, and quantitative computed tomography (QCT) of the lumbar spine, to measure volumetric bone mineral density and to carry out finite element analysis, a method that can assess bone strength. QCT is an extremely accurate method for detecting volumetric bone mineral density changes following intense weight loss.
Research has found that bone marrow fat reacts to nutrition changes and may function as a bone quality biomarker. So, proton MR spectroscopy was administered to patients to assess lumbar spine bone marrow fat.
BMI in the adolescents, as well as the young adults, dropped 2 years after surgery, while there was a slight BMI increase in the control group. In comparison to the controls, patients who had sleeve gastrectomy experienced a significant bone marrow fat increase and a reduction in strength estimates and bone density in the lumbar spine.
It was discovered that bone strength was reduced 2 years following surgery for weight loss, while bone marrow fat, a bone-weakening marker, was elevated, indicating that surgery for weight loss has a negative impact on bone health.
Building bone mass is important in the adolescent years, and bone accrual deficits throughout these years can have a long-term impact on bone health and the risk of fractures in adolescents later in life.
As bariatric surgery is carried out more and more in adolescents, its impact on bone health should be emphasized, particularly to the medical professionals who will carry on to provide regular medical care for these individuals.