About 90% of the risk of peripheral arterial disease, stroke, or a heart attack, can be attributed to smoking, insufficient physical activity, poor eating habits, high blood pressure, abdominal obesity, diabetes, elevated blood lipid levels, psychosocial factors, or alcohol consumption.1✅ JOURNAL REFERENCE
DOI: 10.1093/eurheartj/ehab484
The European Society of Cardiology guidelines focus on artery affecting atherosclerotic cardiovascular disease. There is an inadequate blood supply to the body when fatty deposits clog up the inside of the arteries. This is the main reason behind strokes, heart attacks, peripheral arterial disease as well as sudden death when arteries become totally blocked. Adopting a healthy lifestyle all through life is most important for preventing these conditions, particularly not smoking and treating risk factors.
There are recommendations for healthy individuals, as well as those already suffering from diabetes or cardiovascular disease. Determining who will benefit most from preventative treatments, which includes therapies to reduce blood pressure and lipids, is important for prevention efforts, and so the foundation of the guidelines is the estimation of cardiovascular disease risk.
Blood pressure and blood lipid targets, and glycemic control in diabetes stay the same as in previous guideline recommendations for dyslipidaemias, diabetes, or hypertension. A stepwise approach to intensify preventative treatments is introduced with the current guidelines, while always considering the patient’s preferences, psychosocial factors, other conditions, and potential benefit of treatment. For example, in healthy individuals the stepwise approach begins with recommendations for everyone: following a healthy lifestyle, quitting smoking, and maintaining systolic blood pressure under 160 mmHg. Recommendations are then customized based on the 10-year cardiovascular disease risk (determined by a health professional making use of available risk scores).
Although personalized decisions making use of estimated risk and a therapeutical stepwise approach is more complicated than a one-size-fits-all approach, it’s reflective of patient diversity and is essential for giving each patient the correct treatment.
A new section is dedicated to communicating the shared decision-making process risk. The goals are for people to understand their existing risk and priorities, intervention pros and cons, the anticipated reduction of risk with preventive actions. In healthy individuals, the standard approach is calculating the chance of cardiovascular disease within 10 years. Younger individuals could find lifetime risk estimations and benefits of preventive action more informative, as the 10-year risk for them is typically low.
Quitting smoking is probably the most effective of all of the preventive measures, resulting in significant reductions in heart attacks or death. Smokers younger than 50 have a cardiovascular disease risk 5 times higher in comparison to non-smokers. Stopping should be strongly encouraged for all smokers, and passive smoking should be avoided wherever possible. The guidelines for the first time clearly state that quitting smoking is recommended, and is still beneficial irrespective of weight gain. Although evidence suggests that e-cigarettes could be more effective in comparison to nicotine-replacement therapy for quitting smoking, the long-term effects on lung and cardiovascular health are not clear, and using e-cigarettes together with tobacco cigarettes should be avoided.
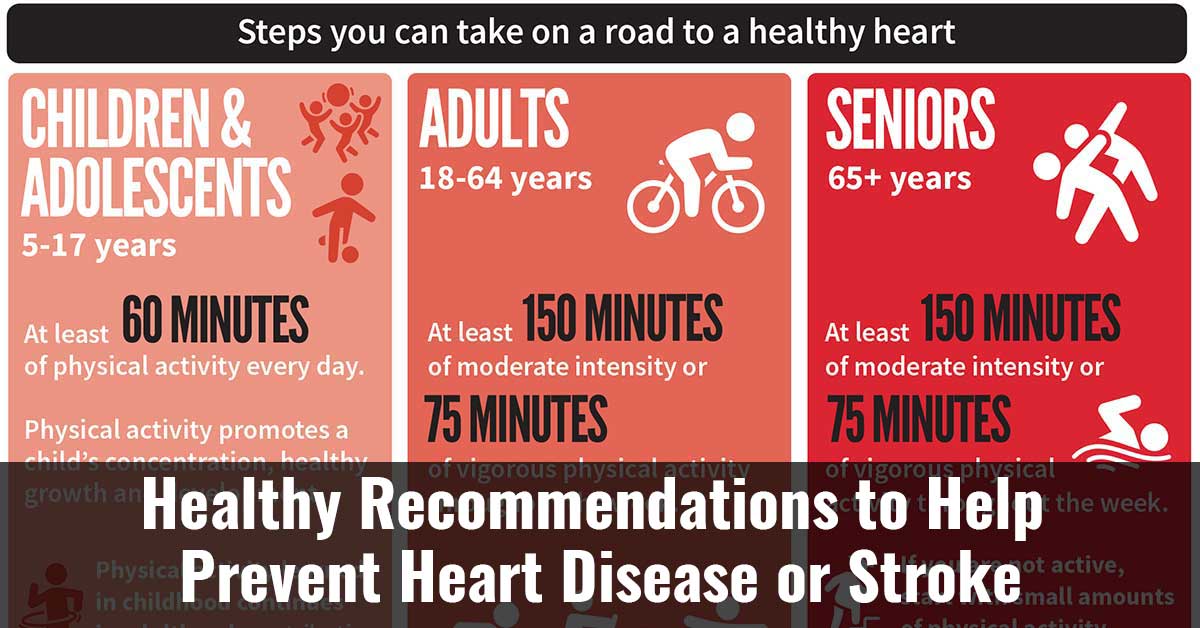
With regards to exercise, individuals should make every effort for a minimum of 150 to 300 minutes every week of moderate-intensity aerobic physical activity, or 75 to 150 minutes a week of aerobic physical activity of vigorous-intensity, or a comparable combination. It’s newly recommended that sedentary time be reduced and to participate in some light activity during the day. Another new recommendation is to consider making use of wearable activity trackers for increasing activity.
With regards to nutrition, the recommendation is a healthy diet is for all people for the prevention of cardiovascular disease. Emphasis should be placed on plant-based foods such as whole vegetables, fruits, grains, nuts, and pulses. Newly recommended is to include adopting a Mediterranean or comparable diet; limiting consumption of alcohol to a maximum of 100 g weekly, consuming fish at least once a week, preferably fatty fish, and restricting intake of meat, especially processed meat.
With regards to body weight, it’s recommended that obese and overweight individuals lose weight to reduce blood pressure, blood lipids, and diabetes risk, and consequently reduce cardiovascular disease risk. The guidelines suggest for the first time that bariatric surgery can be considered for obese people having a high risk of cardiovascular disease when exercise and a healthy diet don’t provide sustained weight loss.
Mental disorders like anxiety are linked to an increased cardiovascular disease risk and a worse prognosis for individuals who already have cardiovascular disease. The new recommendation is to offer more intense support to individuals who have these conditions to improve their adherence to treatments and lifestyle changes. Another new recommendation is to consider referring individuals with cardiovascular disease and stress to psychotherapeutic stress management.
Policy interventions at the population level are recommended for improving heart health and promoting healthy choices, which include air pollution reduction measures, fossil fuel use reduction, and carbon dioxide emission limits. Other measures are better school playground space accessibility, and legislation restricting the marketing of unhealthy food to children on food packaging, TV, social media, and the internet. Marketing controls for addictive e-cigarettes should be similar to those used for standard cigarettes, particularly the varieties that are flavored and appeal to children. Labeling alcohol with health warnings and caloric content can be considered.
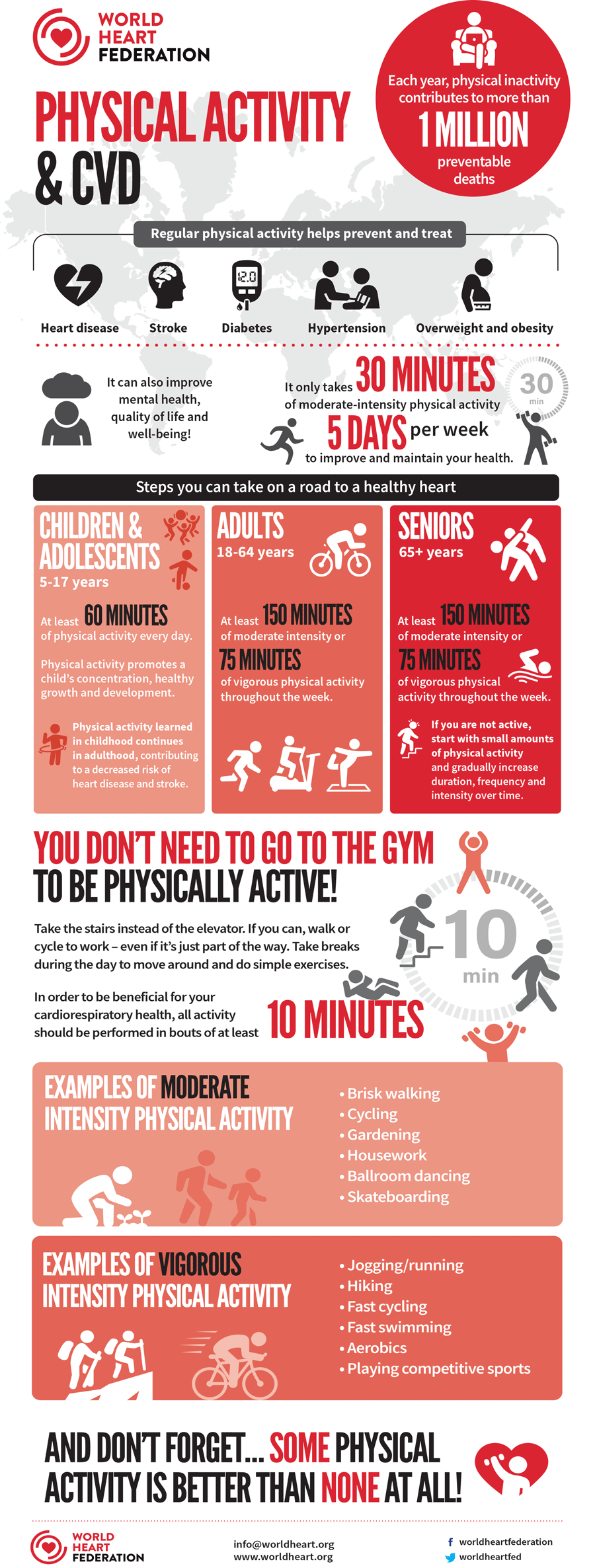
Image Source – world-heart-federation