Research has shown that a healthy lifestyle involving regular social connection, healthy sleep, healthful eating, moderate consumption of alcohol, and regular physical activity while avoiding an excessive amount of sedentary behavior and smoking, lowers depression risk.1✅ JOURNAL REFERENCE
DOI: 10.1038/s44220-023-00120-1
Researchers examined a combination of factors such as brain structure, genetics, lifestyle factors, and the metabolic and immune systems to determine the underlying mechanisms that could explain this relationship.
According to the WHO, about 1 in 20 individuals suffer from depression, and the disorder presents a significant public health burden globally. The factors that affect the start of depression are complex and include a combination of lifestyle and biological factors.
To examine the association between depression and these factors, data were made use of the UK Biobank, a research resource that contains the participants’ health, lifestyle, and genetic details.
By looking at data from nearly 290,000 people, of whom 13,000 experienced depression, followed over 9 years, the researchers could identify 7 healthy lifestyle factors linked to a reduced depression risk. These were:
- Frequent social connection
- Low-to-moderate sedentary behavior
- Never smoking
- Healthy sleep
- Regular physical activity
- Moderate alcohol consumption
- Healthy diet
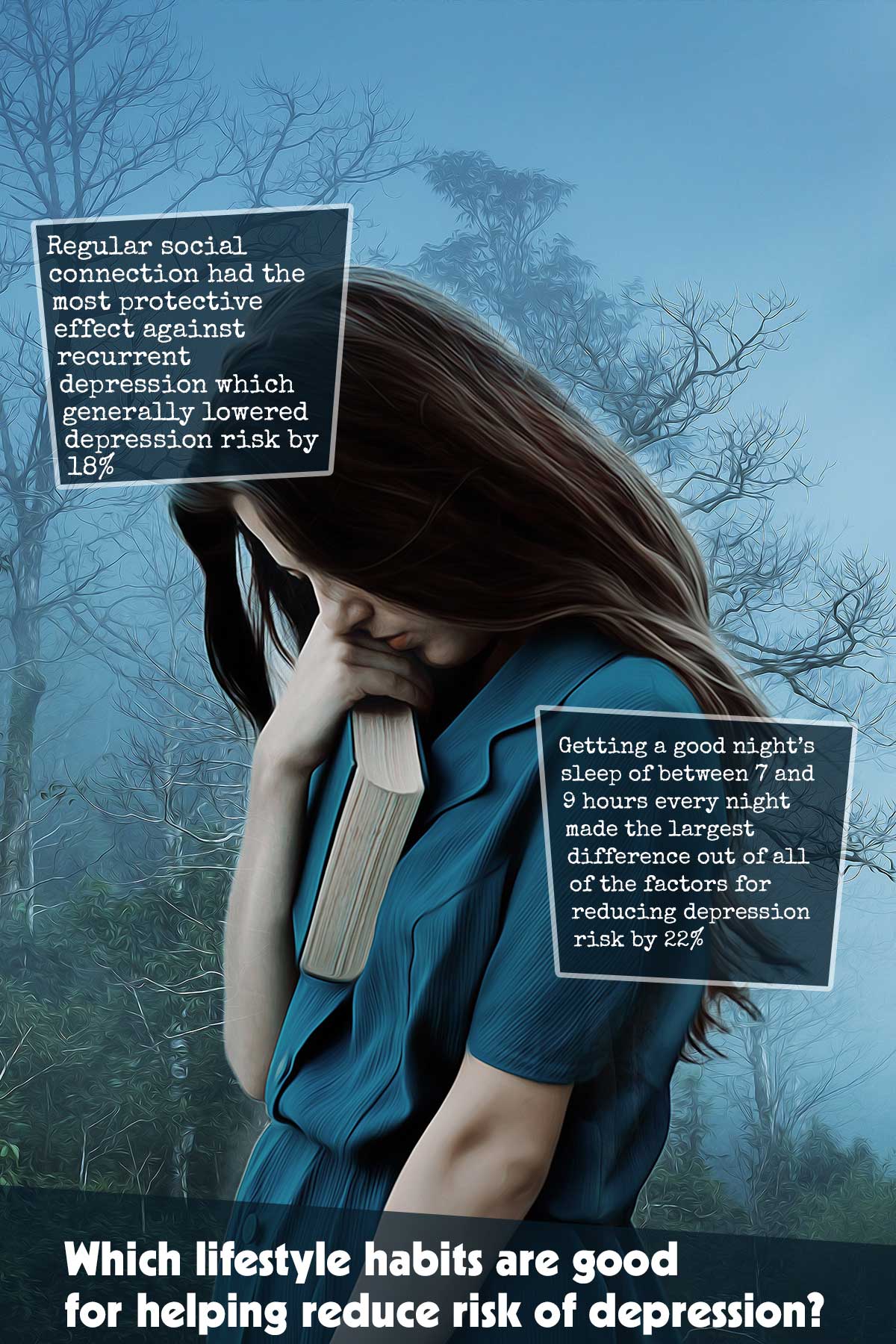
Getting a good night’s sleep of between 7 and 9 hours every night made the largest difference out of all of the factors for reducing depression risk by 22%, which includes treatment-resistant depression and single depressive episodes.
A regular social connection had the most protective effect against recurrent depression which generally lowered depression risk by 18%.
Never smoking reduced depression risk by 20%, regular physical activity reduced risk of depression by 14%, low-to-moderate sedentary behavior reduced risk of depression by 13%, moderate alcohol consumption reduced risk of depression by 11%, and a healthy diet reduced risk of depression by 6%.
The individuals were allocated to 1 of 3 groups according to how many healthy lifestyle factors they stuck to: favorable lifestyle, intermediate lifestyle, and unfavorable lifestyle.
The intermediate group participants were about 41% more unlikely to experience depression in comparison to the unfavorable lifestyle individuals, while the favorable lifestyle individuals were 57% more unlikely to experience depression.
The researchers then looked at their DNA, allocating each participant a genetic risk score based on the person’s number of genetic variants that are known to be associated with depression risk.
Individuals with the lowest score for genetic risk were 25% more unlikely to develop depression in comparison to individuals with the highest score for genetic risk, a much smaller impact compared to lifestyle.
In individuals at low, medium, and high genetic depression risk, the researchers additionally observed that a healthy lifestyle can reduce depression risk.
These results underline the significance of adhering to a healthy lifestyle for the prevention of depression, irrespective of an individual’s genetic risk.
Although our DNA can increase depression risk, the study shows that a healthy lifestyle is possibly more important.
There is a degree of control for several of these lifestyle factors, so looking for ways for improvement such as getting out to socialize and ensuring we get a good night’s sleep can make a difference to people’s lives.
To determine how a healthy lifestyle decreases depression risk, the researchers examined several other factors.
To start with, they looked at MRI brain scans from just less than 33,000 individuals and observed several brain areas where a larger volume, i.e. more connections and neurons, were associated with a healthy lifestyle, which included the amygdala, hippocampus, pallidum, and thalamus.
They then looked for blood markers that suggested metabolism or immune system issues. Among those markers shown to be associated with lifestyle was a molecule produced in the body when responding to stress known as C-reactive protein, and one of the main types of fat that the body uses for storing energy known as triglycerides.
These connections are supported by several other studies. Stress exposure in life can impact how efficiently blood sugar is regulated, which could result in immune function deterioration and accelerate age-related damage to the body’s molecules and cells.
Lack of sleep and inadequate physical activity can damage the ability of the body to respond to stress. Insufficient social support and loneliness have been shown to increase immune deficiency markers and the risk of infection.
The researchers found that the lifestyle to metabolic and immune function pathway was the most significant. So, a poorer lifestyle affects our metabolism and immune system, which subsequently increases depression risk.