According to a study, stress such as discrimination, job strain, traumatic events, and everyday stressors speeds up immune system aging, which potentially increases an individual’s risk of cardiovascular disease, cancer, and illness from viral infections like COVID-19.1✅ JOURNAL REFERENCE
DOI: 10.1073/pnas.2202780119
The study could help to explain age-related health disparities, such as the unequal COVID-19 pandemic toll, and identify potential intervention factors.
Understanding age-related health disparities are important as the population of older individuals in the world increases. Age-related immune system changes play an important part in declining health.
The immune system significantly downgrades naturally as an individual ages, a condition known as immunosenescence. The immune profile of an individual weakens with advanced age, with the circulation of too many worn-out white blood cells and not enough fresh white blood cells available to tackle new invaders.
Immune aging is linked not only to cancer, but to organ system aging, increased pneumonia risk, and cardiovascular disease.
The researchers wanted to find out the reason for extreme health differences among individuals of the same age. They searched for a link between lifetime stress exposure and a decline in the immune system’s vitality.
Enormous data sets were queried and cross-referenced from a nationwide longitudinal study of the family status, marital, health, economic, and private and public support systems of older individuals.
Responses from a sample of 5,744 individuals older than 50 were examined to calculate different types of social stress exposure. The participants answered a questionnaire intended to assess their social stress experiences, such as lifetime discrimination, everyday discrimination, chronic stress, and stressful life events.
The individuals’ blood samples were then analyzed making use of a lab technique known as flow cytometry, used for counting and classifying blood cells as they are passing in a narrow stream one at a time in front of a laser.
Individuals with higher scores of stress had older-appearing immune profiles as expected, with lower fresh disease fighter levels and higher worn-out white blood cell levels. The link between stressful life events and less available T cells carried on even after BMI, drinking, smoking, education, and ethnicity or race had been controlled for.
Some causes of stress could be impossible to manage, but there might be a workaround according to the researchers.
A crucial immunity component known as T-cells matures in the thymus gland, which is located just above and in front of the heart. The thymus tissue shrinks as an individual ages and fatty tissue replaces it, leading to a reduction in immune cell production. Previous research indicates that this process is accelerated by lifestyle factors such as reduced exercise and poor diet, which are both linked to social stress.
The stress and accelerated immune aging association wasn’t as pronounced in this study after low exercise and poor diet had statistically been controlled for. This means that individuals experiencing more stress are more likely to have poorer exercise and diet habits, which partly explains why their immune aging is more accelerated. The immune aging linked to stress can be counterbalanced by improving exercise and diet behaviors.
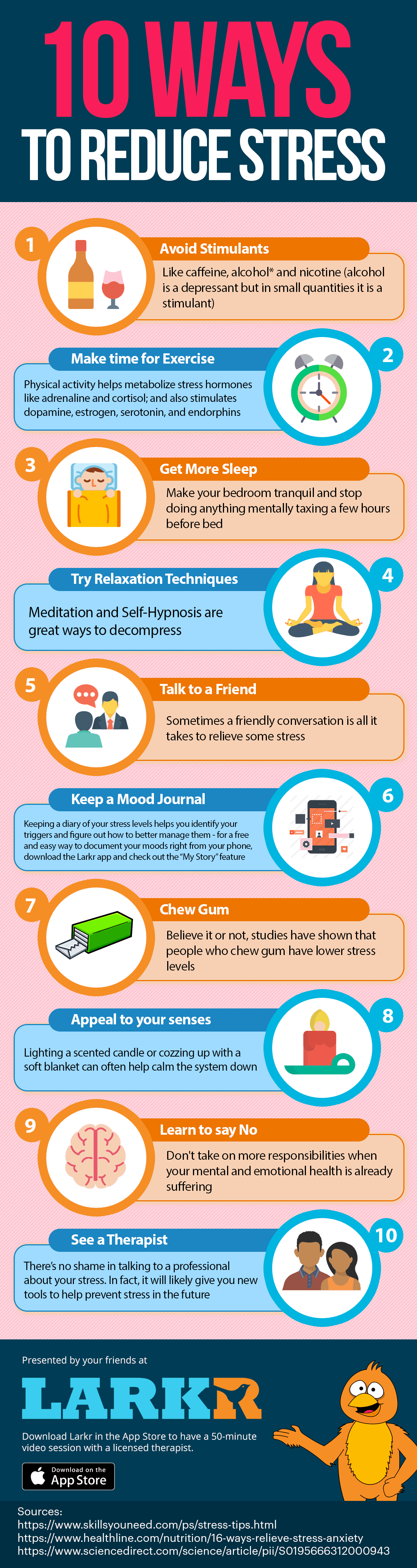
Image Source – larkr



