According to study results, transcranial direct current stimulation may be a non-pharmacological solution to help manage resistant hypertension.1✅ JOURNAL REFERENCE
DOI: 10.3389/fcvm.2022.853427
Resistant hypertension is hypertension that doesn’t respond to extreme medical treatment, characterized as daily administration of a minimum of 3 types of antihypertensive drug (which includes a diuretic) at the maximum tolerated dosages. Individuals with resistant hypertension are at high risk of cardiovascular complications, such as heart failure and stroke.
The impact of a single, acute session or 10 sessions of transcranial stimulation on peripheral and central blood pressure was evaluated in 13 participants with resistant hypertension. The individuals were evaluated for adherence to pharmacological treatment 6 months before the start of the study, as well as during the study, and also for height, body weight, and resting blood pressure, as well as any other medical conditions that might affect blood pressure.
After acute stimulation, 24-hour ambulatory monitored systolic pressure dropped in some individuals by 15 mmHg. A systolic pressure reduction of this degree mitigates cardiovascular risk significantly.
The study results also revealed that the longer transcranial stimulation period didn’t reduce brachial blood pressure, which is measured in the physician’s office on the brachial artery and monitored for 24 hours. A possible explanation is that 10 consecutive days of stimulation resulted in a higher tolerance level and worked initially only, with blood pressure increasing again thereafter.
Prior research carried out by the researchers had shown transcranial stimulation’s potential as a way of modulating autonomic nervous system control and reducing blood pressure in individuals with mild to moderate hypertension, which suggested its potential use for treating resistant hypertension.
The current study was double-blind as well as randomized, which means that the individuals were randomly split into groups and the kind of treatment they were given was unknown to the participants as well as the researchers. It was also a crossover, a kind of study in which all participants are given the same 2 or more treatments in a different order according to the group that they are randomly allocated to.
The 20-minute session effects of actual and sham transcranial stimulation were compared in the acute as well as longer protocols. Individuals randomly chosen for sham stimulation were given electric current just during the first 3 minutes, and the electrodes remained on their skin for 17 minutes in the sham treatment, with the other individuals receiving the stimulation treatment for the full 20 minutes. Following a 1-week break, they were all given 10 consecutive sessions. Following another break, individuals who had been given sham treatment received the full treatment and vice-versa.
The effects of transcranial stimulation were also tested on the autonomic nervous system controlling functions that include digestion, temperature, circulation, and breathing, and consists of the parasympathetic and sympathetic systems, and biomarkers were measured linked to blood pressure, such as cytokines, acetylcholinesterase, noradrenaline, and cortisol.
A hyperactive sympathetic nervous system, which manages responses to stress or danger, including breathing rate, blood pressure, and higher heart rate, is regarded as one of the main causes of high blood pressure and plays an especially significant part in resistant hypertension. It’s linked to the risk of vasoconstriction, arrhythmia, and remodeling of the heart and blood vessels in individuals with resistant hypertension.
Activation of the parasympathetic nervous system, which calms the responses of the body when feeding or resting, has been associated with reduced blood pressure, improved cardiac functioning, and less inflammation.
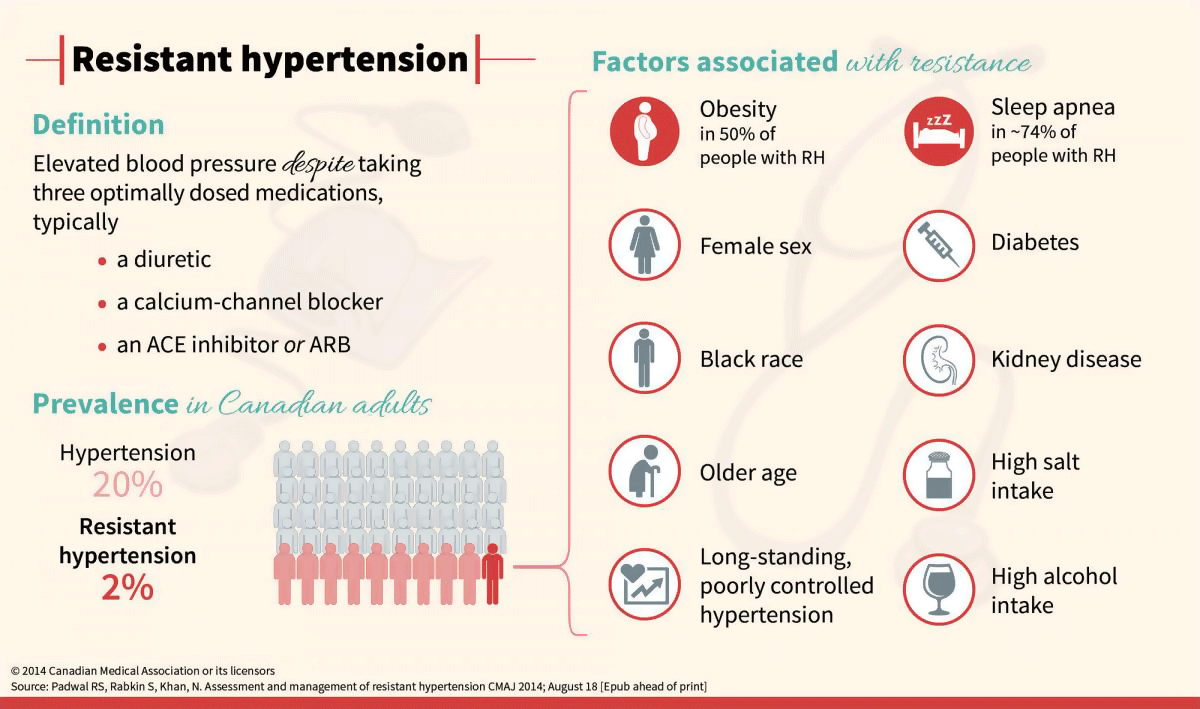
Image Source – cmaj