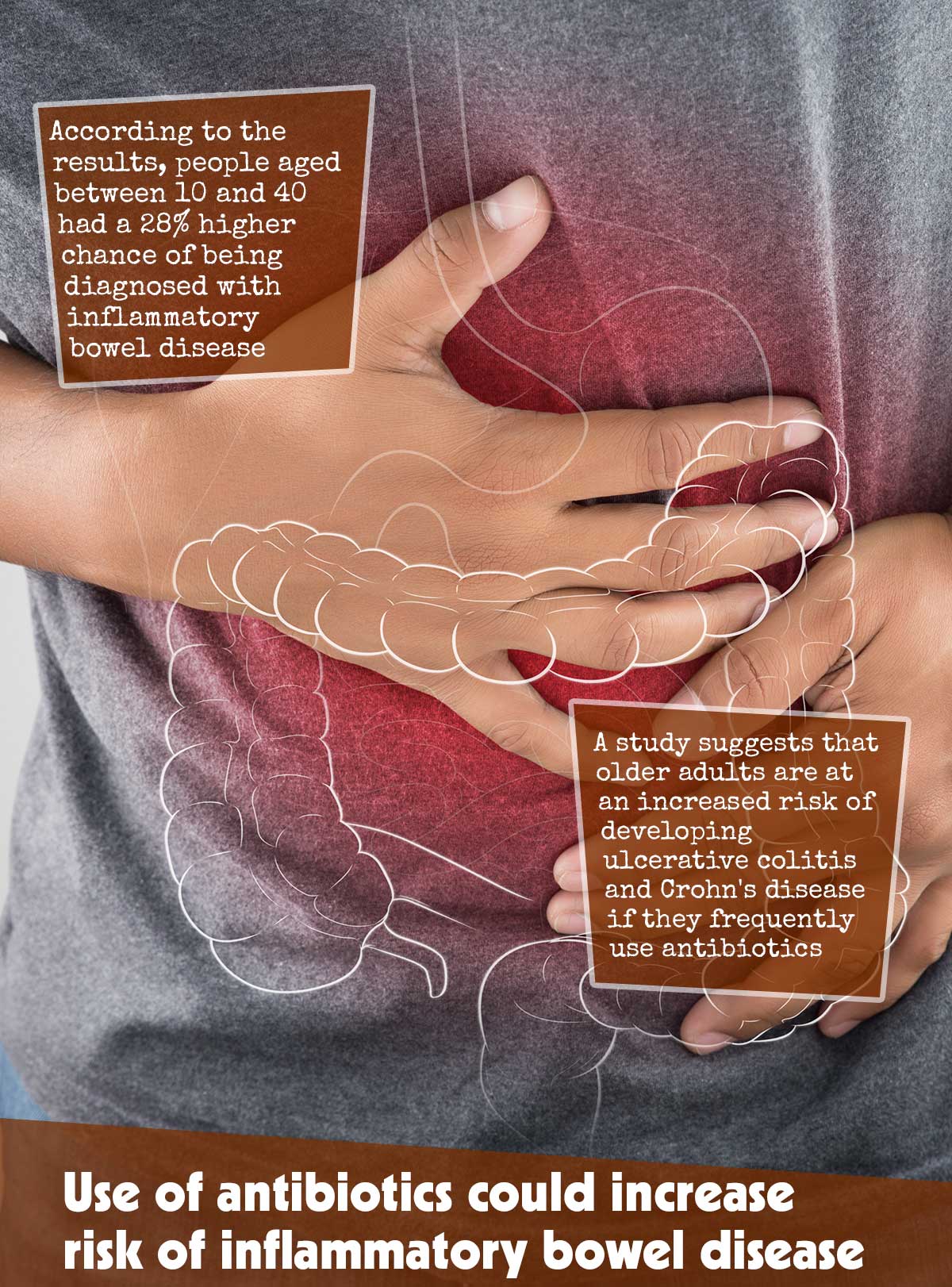
A study suggests that older adults are at an increased risk of developing ulcerative colitis and Crohn’s disease if they frequently use antibiotics. The highest risk is reportedly seen 1-2 years after taking antibiotics, especially those targeting intestinal infections.1✅ JOURNAL REFERENCE DOI: 10.1136/gutjnl-2022-327845
There is evidence suggesting that environmental factors could be linked to Inflammatory Bowel Disease. Currently, there are 7 million people affected by the condition around the world and researchers expect this number to continue increasing in the next decade.
While the impact of antibiotics on inflammatory bowel disease risk among younger people has been established, its implications among older individuals are still a matter of debate. Thus, further research was needed to understand the exact association between antibiotic use and inflammatory bowel disease risk for all age groups.
To deepen the insights on this matter, the research team gleaned from medical records of people aged 10 and over who have no history of inflammatory bowel disease.
The researchers were interested in finding out if the timing and dose of antibiotics could influence the development of inflammatory bowel disease, as well as if this varied between different types of inflammatory bowel diseases or antibiotics.
The study included a total of 6.1 million individuals, with approximately 50% being female. Out of these, 91% were given one or more courses of antibiotics between 2000 and 2018.
Around 36,017 people were diagnosed with ulcerative colitis and 16,881 people with Crohn’s disease during this period.
The results showed that the use of antibiotics can increase the risk of inflammatory bowel disease, regardless of age. However, a heightened risk was observed in older individuals.
According to the results, people aged between 10 and 40 had a 28% higher chance of being diagnosed with inflammatory bowel disease. Those aged between 40-60 were 48% more likely while those over the age of 60 were 47% more likely to be diagnosed with this condition.
The risk of developing Crohn’s Disease was slightly higher compared to Ulcerative Colitis. For individuals aged 10-40, the increase in risk in risk was 40%, for ages 40-60 it was 62%, and those over 60 had a 51% increased risk.
The increased risk each time a course was taken seemed to increase cumulatively. The risk associated with taking each additional course was 11% higher, 15% higher, and 14% higher.
People who receive a course of five or more antibiotics have the highest risk, with 69% greater risk for 10-40-year-olds, double the risk for 40-60-year-olds, and 95% greater risk for those above 60 years old.
The timing of antibiotic usage was found to be a factor that could increase the risk of developing inflammatory bowel disease. Specifically, the risk was highest 1-2 years after the medication was used, and decreased gradually over time after that.
Individuals between the ages of 10 and 40 had an increased risk of developing inflammatory bowel disease within 1-2 years of taking antibiotics, which decreased to 13% after 4-5 years. The equivalent numbers for individuals between 40 and 60 years were 66% opposed to 21% and for those over 60 years 63% opposed to 22%.
The commonly prescribed antibiotics fluoroquinolones and nitroimidazoles used for treating gut infections pose the highest risk of inflammatory bowel disease. Broad-spectrum antibiotics such as these are designed to kill off a wide variety of microorganisms, and not only the ones that cause illness.
In terms of antibiotic types, only Nitrofurantoin wasn’t associated with an increased risk of inflammatory bowel disease. Narrow spectrum penicillins were also linked to the condition, albeit to a lesser degree.
This supports other research that suggests the composition of the microbiota in the gut can play an essential role in health and well-being. Furthermore, certain antibiotics may have a significant impact on this microbial community, potentially causing shifts to its structure.
This research is observational and cannot establish cause and effect. Additionally, there is no available data on the medications taken or how many were consumed by the participants, according to the research team.
The researchers suggest that there could be biological reasons for the results, such as a weakening and decrease of microorganisms in the gut due to aging, which is likely to be worsened by antibiotics.
Also, consistent antibiotic usage can create a more prominent disturbance in the intestinal microbiota, impeding its recovery.